Category: medications
Opiates for pain relief: what patients have to say
My Dr said that she wants to physically see me each month to get my script. I don’t have insurance and can’t afford to do that each month. Our free clinic won’t write for them either… Our health care system sucks! Not sure what I can do though.
I couldn’t function without them. My GP prescribes them. My old rheum would drug test if you wanted him to prescribe. Well, I also smoke marijuana and that would have me booted from the practice altogether. I get them where I can bypass that.
If I didn’t have spousal support/alimony, I wouldn’t be able to afford seeing a pain specialist. It’s so freaking expensive!
A patient in the New York area:
I have only ever been prescribed opiods in the ER or by a GP in a flare. I love my rheum but he doesn’t do pain management of controlled substances because of the current laws and how much more difficult it will make his practice and how many fewer patients he would have because of the increased visit frequency required.
I’m on Diluadid 2mg twice a day. It managed my chronic arthritic pain extremely well at first, but all it does now is make me sleepy. Does it manage my pain? Yes and no. When I’m flaring there is NOTHING that makes my pain go away. Not even high dose pain meds given by IV in the hospital. Nothing. That’s the way my arthritis is. Intractable. So every thirty days I pick up my prescription for a 30-day supply and muddle through another month of trying to manage my pain without really managing my pain!
Since there is no way to know who will become addicted, shouldn’t the focus be on supporting social services that help to check on people living with chronic pain who are on these medications? Shouldn’t we be embracing conversation starters like the recent Super Bowl commercial about Opioid-Induced Constipation instead of making poop jokes & assuming everyone on pain medications is an addict? Should health activists be taking over important areas in other healthcare issues to try to make a point to the Bill Mahers of the world? (Hint: no).
Approximately less than 9% of people who have a substance abuse problem abuse opioids. Some of them are even physicians. What about them? Do they not also deserve pain relief? Our respect, love, and help instead of being vilified?
Terminology Tuesday: Kineret
 |
| I totally stole this pic from Emily @ Chronic Curve |
Well, it’s been done.
I went for labs Thursday morning and, despite a pred boost, my sed rate has only gone down ONE FRIGGIN’ POINT and my CRP has actually gone UP.
I cannot right now with this.
Anyway.
Kineret is an IL-1β inhibitor.
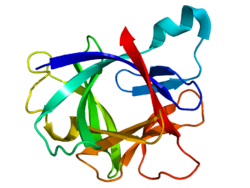 |
| Hi IL-1β! |
This little guy can be a cause of inflammation and in Still’s/SJIA interleukin (IL) medications tend to work better. The theory is that this is the type of inflammation we deal with more than others (TNF alpha, etc).
K-dawg (my new nickname for it) inhibits IL-1β because it’s IL-1α protein which can block the beta bits from attaching to cells and causing inflammation.
Some of the studies with Still’s show symptom relief within HOURS which is pretty friggin’ baller.
The downside? Well there are a few.
It’s still a biologic and it still inhibits the immune system. I haven’t had as much of a problem catching the ick from people on TNF drugs, but that can be a sign that those drugs aren’t working for you. The nice thing right now is that I share an office with one person AND work with docs, so they’ll totally get my precautions.
K-dawg is injected daily, which is nice if you have to stop it for some reason but annoying because daily shots.
The other big downside? Major injection site reactions. They seem to last for like a month for most people, causing fun painful welts. I’m not excited about this, especially if I do end up starting here before my JA conference trip and my previously planned swimsuit time while there.
Oh well.
I’m trying to look at it in a good light. With my old rheumy, I’d be stuck moving onto another medication that wouldn’t really do much for me. This is why I switched docs. With my current rheumy, who has treated Still’s before and hates step therapy, I’m ready to really deal damage to Arthur.
| /nerd |
I’m also hopeful. None of the medications I’ve been on would get me to remission. This could. And that’s an awesome notion.
Therapeutic Thursday: physical edition
I haven’t done my Cimzia shot since… um… like the beginning of March? Maybe earlier?
Yeah…
Part of it is that I had bronchitis and had to skip a shot for that, and then I was out of the state for Sam’s surgery and my shot was not even close to the top of my priority list.
The other side is that, of course, it’s not working well anyway.
It’s hard to admit, but there it is. I end up with side effects for 3-7 days, have an okay week, and then just have to inject again. It’s counterproductive to have a shot that causes more problems than it solves – and this hasn’t done well at all for reducing my inflammation.
I had labs when I got back from Cali that showed an increase in my CRP and my sed rate – even from when I had bronchitis. Clearly, even though I feel well right now, I need to have a medication.
One of the reasons I switched to this rheumy in the first place was because my old rheumy’s office would not consider the SJIA/Still’s specific medications like Actemra or Kineret for me. It was frustrating to know that there were medications out there that would likely help me more and they instead put me on a third TNF drug, which is not very common. They generally move on to another class once two of a certain class of drug has failed to work for you.
The rheumy asked, via MyChart, if Kineret would be something I’d be willing to do. I sent back a short list of meds, and she sent back more info on Kineret. It sounds like that will likely be my next step.
The thought of going from bi-weekly shots that I dreaded to daily shots doesn’t quite have me enthused… but in comparing the drugs I suggested, this one does look as though it will be the best for me for what I need right now.
So today, I get to meet with my rheumy to discuss… and then have a meeting with my therapist right after to prevent the mental breakdown that almost always seems to accompany a change in medications.
It’s a good change, but it’s another point where it feels like I’m a failure. I know logically that the medication has failed me, but lingo always points to the patient failing the drug.
Cimzia was never going to get me to remission. It helped mildly for a short time, but wasn’t in it for the long haul, and that’s okay. Kineret could be, for me, a shot at remission. I’m willing to deal with the risks, to put up with mild injection site reactions and daily shots, for the chance at a more normal life.
Terminology Tuesday: DMARDs (and a warning about antibiotics and C. diff)
DMARD stands for Disease Modifying Anti-Rheumatic Drugs. These drugs help to slow the effects of rheumatic diseases and are often the first lines of defense against further joint damage, especially in adults.
DMARDs include drugs like methotrexate, plaquenil, minocycline, arava, sulfasalazine, imuran, cyclosporine, xeljanz, and the biologics (Enbrel, Humira, Cimzia, Kineret, Orencia, Rituxan, Remicade, and Simponi).
These are likely drugs that you’re used to hearing about. For children diagnosed with juvenile arthritis, they often try to stick with an NSAID first (check out next week for more information on that term). Steroids can also be used, but should be used more in the short term to limit side effects.
Someone with a rheumatic disease can end up on a combination of several of these medications, all of which impact your immune system. Steroids even do that!
Many of these drugs are used for other diseases as well, from autoinflammatory/autoimmune to cancer to more.
Rituxan, Remicade, and methotrexate are all used as treatments for some types of cancer in higher doses than a rheumatic patient would receive. Minocycline is an antibiotic, but has been used to fight RA and related diseases. Treatment with antibiotics doesn’t work for all and there can be serious risks in that treatment, including C. diff which is horribly painful in addition to easily transmittable and potentially fatal.
I had C. diff in July of 2012. I let it go for nearly two weeks before doing anything because I thought I was just sick to my stomach or had food poisoning. The process to diagnosis involved collecting my own ‘output’ and taking it to the clinic.
So gross.
Honestly, with how long I let it go, I’m lucky that I didn’t end up in the hospital – and that I didn’t give it to my pregnant-at-the-time sister!
Moral of the story? Don’t take antibiotics unless you have to.
Reflections on 21 Years of Illness, Part 2: New Medications
This coming Friday will mark 21 years of living with this disease for me. It’s not necessarily a day I want to celebrate, but it is also a day that I cannot let go by unmarked. I hope to write a few different blog posts this week reflecting on the live I’ve lived so far, the lessons learned, and the amazing steps that have been made in chronic illness and rheumatology care since 1993. This is part two in the series, documenting the breakthroughs in rheumatology over the last 21 years.
Enbrel [TNF alpha inhibitor]:
Approved to treat RA (Nov 1998)
Polyarticular JIA (1999)
Psoriatic Arthritis (2002)
Ankylosing Spondylitis (July 2003)
Plaque psoriasis (April 2004)
Kineret:
Approved to treat RA (Nov 2001)
While not FDA approved to do so yet, this is a drug of choice for SJIA/Still’s
Humira [TNF alpha inhibitor]:
Approved to treat RA (Dec 31 2002)
Psoriatic Arthritis (2005)
Crohn’s Disease (2006/2007)
Orencia [T-cell inhibitor]:
Approved to treat RA (Dec 2005)
Cimzia [TNF alpha inhibitor]:
Approved to treat Crohn’s (Apr 2008)
RA (May 2009)
PsA (Sept 2013)
AS (Oct 2013)
Simponi [TNF alpha inhibitor]:
Approved to treat RA, PsA, AS (Apr 2009)
Ilaris [interleukin-1 beta inhibitor]:
Approved to treat CAPS (Oct 2009)
SJIA (May 2013)
Actemra [interleukin-6 inhibitor]:
Approved to treat RA (Jan 2010)
SJIA (Apr 2011)
Polyarticular JIA (Apr 2013)
New SubQ form approved for RA (Oct 2013)
Xeljanz [JAK (Janue kinase) inhibitor]:
Approved to treat RA (Nov 2012)
As you can see, there has been a ton of improvement in medications in the last 21 years. In 1993, the go-to was methotrexate if you weren’t going to go into a medical trial for one of the above medications (namely Enbrel).
With these new medications, we have a better chance of finding a medication that works for each patient. We also have more options for harder to treat patients, especially those of us with SJIA/Still’s.
An update on my medications, or why I’m breaking up with my primary care doc
I haven’t done my Enbrel shot for like a month and I hate that.
Oh come on now, it’s not like this was my plan.
Earlier in the year, I developed a mucocele just to the right of the middle of my palate. I was nervous and thought I should see the dentist but clearly did not. At the beginning of May, the mucocele was still there and I developed a cyst above my upper right canine along the gum line but also so big it was up next to my nose. When it didn’t go away after a week-ish and actually was beginning to swell to the point that it was impeding my work, talking, and drinking alcohol at trivia, I decided to make an appointment with my primary care doctor. I had held enbrel already hoping for this to go away and I probably should’ve gone to the dentist in the first place, but I never thought I’d experience what I have in the last month.
He feels my face for differences between the right and left side and apparently feels nothing. He sits back and WHILE LAUGHING says “I think it’s just a pimple.” I then go into explaining that I’m 25 and I’ve had my share of pimples but this isn’t a pimple. I explain that it is affecting my job, how moving those facial muscles at all is incredibly painful. I invite him to mash my face again. He goes to town, mashing incredibly hard and even my left side is in pain and by the time he’s done he says, “Well, it clearly doesn’t hurt that bad because you’re not reacting.”
Okay, by this point I’m pretty pissed and I figure he’s already laughed at me so all bets are off the table really but I’ll still be civil. My laughing along with the comment, “Well, you’re talking to a chronic pain patient who pretty regularly sees 8s and 9s on the pain scale so that doesn’t hold as much weight as you think it does,” is met with no response. I would’ve offered to have him look in my mouth but it’s pretty obvious he thinks I am an idiot. He moves on, reassures me that it is a pimple and I’ll feel better when it comes to a head, tells me to take my enbrel, and gives me a week-long script for an antibiotic – which he is only giving because I protested because he warns me AGAINST taking since I had C-diff last year.
I walk out pissed beyond belief that I can’t even fathom what has just happened. He’s always been a bit off and seemed to dismiss a lot of what I have gone through or am going through when he sees me. While I had C-diff, he gave me ten oxycodone pills because I basically broke down in his office since I had to hold enbrel and my normal meds were not going well because of the infection – and that’s after he prescribed me something I was allergic to at first, necessitating me driving all the way back over town to pick up the script.
I make it to the car and it takes all my resolve to open the door and get in the car instead of going back in and going off on him. I sit, unable to bring myself to start the car, and just sob uncontrollably. I don’t even know what to do. I drive home, continuing to sob, and manage to stop enough to get into the apartment before going off again.
One of the worst things that happens with these diseases is when you aren’t believed – that goes double for family members and doctors. My primary care doctor thinks I’m a hypochondriac, a young girl who knows nothing about her own body or medicine. I would’ve expected something like that out of someone much older than the 30- or 40-something man that barely sees me.
I hold my enbrel, despite the incredible amounts of pain I stumble upon in the almost two weeks until I see a medical professional again – but this time it is my scheduled visit with my rheumy’s NP who is the sweetest, most caring person I’ve ever met. I know that, whatever I have going on with me, she’ll know what to do.
My appointments with her are always pleasant, no matter how much I hurt, and I always look forward to them. We sit there, like a couple of River Song clones with our big fabulous hair, and discuss my wedding plans, seeing Wicked, and how I think I’m doing right now compared to last year when I started enbrel. I talk about running and about my fitness regimen that I keep up myself now without PT. She’s so happy. I fully intend on mentioning what has gone on, but I wanted so much to have an appointment with her that wasn’t full of problems.
“So, no more infections?”
Sigh.
I go into the whole thing – what makes this worse and how nothing seems to make it better, and that I’ve been off antibiotics for almost a week. She finally looks inside my mouth to find my lovely sac o’ pus. We discuss my financial state and how without the enbrel I feel terrible – my right shoulder has just started going off, a great sign of a flare for me that only gets worse. I am to update her in a week and if this thing isn’t gone go to a dentist asap. She goes into some more detail on how bad abscesses can be and what they will do to my ability to take DMARDs for, oh, a few months if left alone to fester – or worse. Did you know abscesses can kill??? She leaves me with a hug and reassurance that I did the right thing, along with the name of the primary care doc who she and her husband both see so I can make the switch.
“Hold the enbrel until all signs of infection are gone” are not words a girl in a flare – Kathy noticed the puffy joints – want to hear.
All week I am in agony and freaking out. The right side of my face is killing me with itching, and my arms are trying to finish the job. I have essentially had my arms more or less frozen at my sides, in typing mode. I have to wear my regular bra because even thinking about the sports bras hurts to high heaven. I have a terrible time getting dressed and doing my job. When it isn’t busy, I cry while reading pretending that book is the reason. This pain won’t stop and I can’t take it anymore.
June 6th arrives with only minimal lessening in this sac that I can’t seem to stop playing with. I’m scared to death I’m going to pop it and melt or something. I make a call in the morning to the dentist office I love but haven’t been to in almost two years due to low funds. I set up an appointment for the 7th.
Judgment day arrived today. I’ve known from the beginning that this was an abscess and that I would either be missing a tooth or get a root canal. I knew it and I’ve known that was what I should do all along, but of course I didn’t. I’m there 5 minutes and the x-ray confirms what I’ve thought for a month, but didn’t follow up on because my GP made me feel like shit about myself.
Turns out, my dentists had a cancellation right after my appointment and could do the root canal right away and since I now have dental insurance I owe less than $500. In an hour and a half, my root canal was done and the most painful part was numbing up my gums. I feel fine, mouth wise now. The rest of the infection should be cleared up within a week – if it’s not I get to call for more antibiotics. So best case scenario I’ll be away from enbrel 6 weeks total – worst 7 or 8.
I plan on writing a note to my current GP about the situation and my distaste for his wanton disregard for my safety, knowledge, and experience. I just don’t know what to say exactly – “Thanks fucker, you were wrong and go fuck yourself!” seems a bit much.
This all just goes to show that we know our bodies much more than others do. When we know something is wrong, we’re generally right. Don’t silence that little voice in the back of your head, because it could end up saving your life.
2012: A Year in Review
2012 was an… interesting year for me. It’s not like it was horrible – and yet there were definitely times it was. It has been a tough year.
In January, I officiated a wedding between two good friends. It was wonderful to be a part of their special day. I always knew they would end up together. I also had a good ophthalmology appointment, thankfully, after dealing with some more uveitis off and on in the end of 2011. I also started MTX injections to see if I could handle them better than the pills to help boost Humira. It seemed like it was okay, until the back spasms that still plague me today started and the MTX had too much of an affect on my energy levels and my body function. I was coming to terms with the fact that this semester would be my last in graduate school, as my illness was worsening enough to cause too many problems.
In February, I learned that I was on the verge of getting fired because of misunderstanding poorly explained attendance policy information at work. I brought a note from my rheumatologist about the flare up nature of my disease and stated that I shouldn’t be in as much trouble as I was because I wasn’t missing days to go dick around or go to concerts – I was missing days with illness. I got to play the waiting game. I also saw a PT a number of times for my left knee and back.
With March came the JAM walk in Minneapolis at the Mall of America. We took a long weekend and drove up there, enjoying experiencing the shopping and food nearby. I also had been taking Arava instead of the MTX – but even with that, Humira was definitely not working.
By April, I had run out of my free shipments of Humira from Abbott anyway and it was as good a time as any to make an appt with my rheumy about switching to Enbrel. Even though we decided on switching in April, it would be May before I could start it. I set up a new GP since having one at the university I was no longer attending wasn’t helping anything. I also got to see one of our favorite musicians, Eric Hutchinson, right before my birthday.
May brought with it another arthritis walk, where my sweet boyfriend got an ‘arthritis hero’ sign for me. Doing the whole walk was really tough, as my hips were definitely not excited about a 5k. I had a bone density test, which came back perfectly normal. I participated in the first ever World Autoimmune Arthritis Day (WAAD) by preparing a number of documents and a presentation on living life to the fullest with autoimmune arthritis. The same weekend that was going on, the fiance and I got to go try out for Jeopardy. I have literally been training for that since I was very little and it was great great fun to be a part of it. I had to stop Enbrel after my first injection for about a month due to a sinus infection that got so bad as to swell my entire face. At the end of the month, my rheumy’s NP cleared me for Enbrel again and I got to spend some time with a few friends in town running a marathon… which turned into a half instead because of the horrible hot spell we were having.
By June, dealing with the mental issues of having an illness caught up with me. Though I wasn’t suicidal by any means, I was having thoughts that scared me and I had my first appt with my therapist. The Enbrel was working well enough that we decided I should try it without the Arava as it was upsetting my stomach. The boyfriend and I also went on a wonderful vacation, seeing some sights associated with the Civil War and Abe Lincoln, taking in a Cincinnati Reds game, and meeting one of the best spoonie friends I have ever had. I was able to do so much more physically than I thought I would because of the Enbrel. I also had some dental work done.
As a result of that dental work and taking antibiotics as a precaution, July saw me dealing with C-diff – an infection that is one of the leading killers in hospitals every single year. I dealt with it for 11 days before seeking treatment, thinking it was just salmonella or food poisoning. I am very lucky I got better and didn’t have to face hospitalization. I did drag the boyfriend to Urgent Care on his birthday though, and scared the crap out of him when the nurses came to get him to bring him back to the exam room where I was getting my first IV of fluids due to terrible dehydration. This meant another month with no Enbrel. I got to see Dave Matthews Band, one of my favorites since I was little. I could’ve done without the copious amounts of drugs being done around us but it was neat nonetheless. I went with my sister to her last prenatal visit, and tried to talk to my GP about pain meds. He sent me home with ten pills total. UGH. But I also got a nice haircut and color, and saw the new Batman movie all by myself.
August started off with a bang. On the 1st, I was lucky enough to get to be around for the birth of my niece Marissa Mae. I got to spend time with my best friend when she came along with the boyfriend and I to the Irish Fest Arthritis Walk in Milwaukee. I wasn’t able to walk all of it and almost had to break out the cane to retrace my steps. It was a tough tough day. The next day though, I got to see my idol Hugh Laurie in concert playing the blues. It was one of the most amazing things I have been able to do. I cried out of happiness and being moved by his music. We finished the month off with a Milwaukee Brewers game and spending some time with the boyfriend’s dad.
And then came September. We started the month off with a friend’s wedding and then having to miss Marissa’s blessing because of horrible fibro and rheum pain. It was a horrible day pain wise, but even worse knowing that my family maybe didn’t understand and thought I was an atheist freaking out about going inside a Mormon church again. We went to a Juvenile Arthritis Family Network meeting, along with Megan and Mia and Megan’s sister who deals with AS. It was wonderful to get to meet them after talking so much with them since June when Megan found this lovely blog. I had an appt with my rheumy’s NP, only to get diagnosed with fibromyalgia on top of my Still’s. On the 20th, the boyfriend and I had our 5 year anniversary and headed out to Dubuque to celebrate for the weekend, where he proposed 🙂
In October, I got to spend some time with my best friend and now maid of honor. I was also finally granted FMLA at my job which has made things a lot easier. I babysat Marissa for a while so my sister and her hubby could go out on a date for their one year anniversary, and we found out Marissa likes ukulele music.
November was a hellish month though. I had four appts between the 8th and 9th, one of which was a sleep study. I had to stop Enbrel AGAIN (seriously??) because of an issue with my throat and all doctors involved not wanting to see that end up as an infection. I gave a speech at an Arthritis Foundation fundraiser and got a hug from a Heisman Trophy winner. I also celebrated the 19 year birthday of my Still’s on the 14th and we made a cake. In two years, I am having a 21st birthday party all over again I swear. I also started seeing 2 PTs for my neck/spine, one being pool based therapy.
December has been an incredibly tough month. Cold weather always makes Arthur an ass, and it is definitely doing so now. I’m mid flare as I type this even. And what’s worse for sure is losing someone that I was so close to, that always had ideas and advice and help even if she was going through worse. Losing Laura has made the rheum community come together in a way I have never seen before. She was truly an angel and I am grateful that she isn’t hurting anymore, but I am so sad not only for myself and our other friends but for her fiance and families. As so many others have put it, her death makes me feel numb and I know that I am having a hard time dealing with it. There is a void left by her absence that will never be filled.
While I was lucky enough to go through some amazing once-in-a-lifetime kinds of things this year, I am ready for it to be over and to start anew. Dear 2013, bring a bunch of kick ass things like 2012 had but can you leave the crappy parts behind? I could really really use a break.
So you have a dragon: living with Still’s Disease
Hooray for dragons!
Dragons are elusive creatures, but when you find one you have to really put your all into the fight. It’s no wonder why Still’s Disease is also referred to as ‘the dragon.’
As of 2023, Still’s Disease is one label that covers what was formerly known as systemic-onset juvenile idiopathic arthritis (SJIA) and adult-onset Still’s Disease (AOSD).
I live with SJIA and have since mid-November 1993. Honestly, I barely remember what it was like to be ‘normal’ but I consider this a gift. I’ve watched so many people be completely blindsided by a diagnosis later on in life after they’ve established running or weight lifting as their favorite activity. Watching them struggle with learning their new limits just breaks my heart. I didn’t have to go through that falling ill at 5 years old – I learned my limits while I learned how to do normal things. My limitations, for the most part, are about what they have always been. I am very lucky.
So what is Still’s anyway?
SD is a form of autoinflammatory arthritis that is named after a pediatrician, Sir George Frederic Still. His doctoral thesis was actually about Still’s, and he was the first to describe the phenomenon. He noted that the children afflicted with the disease not only presented with arthritis but also high-grade fevers and a funky rash. Over the years, people starting also noticing these symptoms in adults, thus ‘creating’ Adult-Onset Still’s Disease (AOSD) as a classification.
About 95% of children with this condition present with the rash but only 85% of adults do. The rash can itch, or it can just be there. It also seems to present more with the fevers, though the rash can be brought about manually – by clothes, rubbing against things, and even hot temperatures and water (i.e., showers).
 |
| This wasn’t post shower, but you get the idea. |
What do you mean by autoinflammatory arthritis?
Instead of filtering and removing toxins, the system instead can introduce even more crap at any given point into the system. Think of it like a combination garbage and milkman but very confused. He should have called into work. Instead of leaving healthy milk and removing garbage, this dude gets all turned around. He misses stops, drops off garbage instead of picking it up, and steals all the milk. Here’s the best part – since the lymph system involves bone marrow, blood, lymph fluid, and more, there is no point of refuge from this guy. No spots are left untouched.
Your body keeps getting these messages that something is wrong, and sends T cells and white blood cells out to protect and serve. They’re on like super-secret protection status, like a super protective parent. Anything that a normal person might do – like running for example – is seen as a huge problem. Your immune system says “Whoaaa, hold up there! We got an invasion on our hands!” and calls for reinforcements to protect your knee… but then they get there with all the troops and the only thing there to attack is the knee itself. Swelling leads to immobility of the knee, which can be painful because then you rest the knee not realizing that the knee is a self-lubricating joint – resting too much then makes it hurt more.
Voila, welcome to joint damage!
Treating this disease
It all sounds kind of easy to explain, but the problem in finding the best, most effective treatment lies in what causes the immune system to freak out. And this brings us the different classes of drugs we have to treat different kinds of arthritis, from TNF alpha inhibitors to interleukin inhibitors to chemotherapy medications.
 |
| Mmm bio-hazards. |
As of 2020, there are a few medications approved to treat these conditions. There was only one medication actually approved by the FDA to treat Still’s as of 2012 – tocilizumab or Actemra. It is an IL-6 inhibitor given by infusion usually about once a month. Thankfully, there are a few other options. Canakinumab (or Ilaris) is a newer medication that targets the IL-1 beta protein. It’s usually given by injection once a month or so. Anakinra (or Kineret), another IL-1 inhibitor, is given by daily injection.
Some people respond well to other arthritis medications such as Enbrel, Humira, Methotrexate, and others. That’s especially true in combination with one of the above medications.
Some very very lucky people get to experience remission with Still’s. However, the only statistic I have found – specifically for AOSD – isn’t very comforting. Only about 20% are expected to reach remission. Even then, once you get there, you might not keep that for very long.
There are a number of theories for how to make a ‘cure’ for autoimmune arthritis diseases, probably the most common one involves the use of stem cell therapy. There have been a couple of small studies done with stem cells in other countries, obviously, due to odd feelings about these cells in the US. A large percentage of people experienced a flare-up and worse disease from the process while a slightly smaller number did achieve eased disease activity – for how long is yet to be seen. A very small portion… died. The process is very involved and difficult for the body to go through.
While I maintain hope that stem cells may hold the answer to kicking this disease’s butt, the odds are just not in our favor right now.
Living with this
I’m not going to sugar coat it and say that living with Still’s is easy or awesome because it is entirely too far from the truth. With the right mix of medications, physical therapy, and a great support system, living with this condition can be manageable.
In 2015, I started Kineret. As of the end of 2023, I’m still on it. It’s done wonders to help control the symptoms I experience. In fact, it’s done so well that I sometimes miss my SJIA symptoms. That’s a head game I never thought I’d play.
The best advice I could give someone with this condition would be to value yourself. It is so so easy with how society treats disabled people for us to devalue ourselves. Ableism is a vital thing to learn about and unpack.
Learn as much as you can about this condition. Figure out what you need and want out of life. Then try to think about how to make that happen. I play hockey and perform burlesque now, two things I never thought would be possible.
Oh Enbrel, Where Have You Been All My Life?
I have had kind of an amazing day in general. I picked up my ukulele again after a week of craziness.
Someone got to go get their Enbrel today from the pharmacy. I was super excited. I drove home. I blasted some ‘At Last’ by Etta James. I may have danced around in the living room with my Enbrel package.
I’m sorry you guys, I didn’t manage to take pictures of that. Super lame.
I took my time with it tonight and finished a lot of thing I’ve been meaning to do. I made mac and cheese from scratch, folded laundry, and even cleaned up around here! Whoa!
I pulled out the Enbrel pen from my little package and grabbed my ice pack from the freezer. Then, I settled in for a lovely bit of light reading. I actually read all of the information that comes with the pens.
I feel like maybe if I had read all of that when I started Humira I would maybe have rethought my decision. I don’t care that it’s less than a tenth of a percent, I don’t like knowing the anti-TNFs have caused multiple sclerosis in some people. I mean, what the fuck? I watched my great grandma die from that and now I gotta worry about that from a med? FUCCCCCK YOOOUUUU LIFE’S HEALTH CARD.
But okay, whatever. I’ve been on Humira for like a friggin’ year. So I mean, I might as well keep going.
I had been told I was getting syringes and so didn’t feel like I needed a teaching because it’s like injecting MTX. I actually got the sure-click auto pens. Maybe it was an insurance thing? Oh well, whatever.
 |
| My pen and my handy dandy how-to sheet |
Once I figured out how to use the pen, the shot was so quick. It was so painless. I was able to watch the plunger on the pen push the solution into my body, which I think helped as a distraction. I also was hanging out for like half an hour reading all that shit before injecting while icing my belly. The needle felt so much smaller than the Humira needles. They were so much more gentle. How come you guys never told me???
I’ll keep you guys all up to date with how this goes. I really feel like it could really be something amazing for me – and maybe for you or your loved one.
Enbrel, I think you and I are going to be a great fit. Help me keep that bastard Arthur away and I’ll always keep you in the fridge in my heart.











